The Authority has been a keen advocate of reforms to health professional regulation. Our thinking outlined in Right touch regulation built on the principles of better regulation and laid the basis for a simpler, more proportionate risk-based approach within health and care professional regulation.
In 2015 we published Rethinking regulation which called for radical change for professional regulation, underpinned by right-touch regulation principles, to better the support the significant changes proposed for the health service.
Regulation rethought, published the following year (2016) expanded on our thinking about what needed to change within the system highlighting the complexity and the challenges faced by patients, professionals, employers, educators, and those involved in workforce development. In Right-touch reform published in 2017 we laid out a detailed set of proposals for reform covering both short-medium term improvements and a longer-term vision for change built around proposals for a single regulator common code of practice for all professionals and overall a more coherent regulatory system.
Simplifying regulation is long overdue in the UK but what are the benefits in practice?The Authority has been a keen advocate of reforms to health professional regulation. Our thinking outlined in Right touch regulation built on the principles of better regulation and laid the basis for a simpler, more proportionate risk-based approach within health and care professional regulation.
We were delighted to see the Government echo many of the Authority’s proposals for change in its 2017/18 consultation on reform Promoting professionalism, reforming regulation and to see reforms to regulator powers and governance progressed through a further consultation earlier in 2021 with the intention to take forward changes to each regulator in turn starting with the General Medical Council next year.
However, the Health and Care Bill presents a new opportunity to look at significant structural change to what is generally considered a complex and confusing system. We have commented on the proposed powers for the Secretary of State to merge or abolish regulators and the ongoing review by KPMG looking at options for reconfiguration in our recently published report Reshaping regulation. In this report we reaffirm our view that a single regulator would be the best way to address many of the outstanding problems in the current system and make the whole system work better for all but particularly for patients and the public.
But what are some of the benefits where a similar model has been introduced in practice? In Australia, the National Registration and Accreditation Scheme was introduced in 2010 bringing in a new system for regulation of health and care professionals. This included the creation of the Australian Health Practitioner Regulation Agency (Ahpra) which took on a number of the functions of professional regulators and which works in partnership with the 15 national professional boards. In our guest blog, Chris Robertson, Executive Director of Strategy and Policy and Chloe Moss, National business Coordinator of Strategy and Policy at Ahpra outline some of the benefits that they have found from introducing such a model in Australia. At the end of the article, they do note briefly some of the drawbacks of the single regulation scheme, and we should recognise that what works in Australia will not necessarily work in the UK – but it is definitely worth bearing in mind as we look at opportunities to reshape regulation.
Key benefits of the Ahpra style model
Establishment of the National Registration and Accreditation Scheme
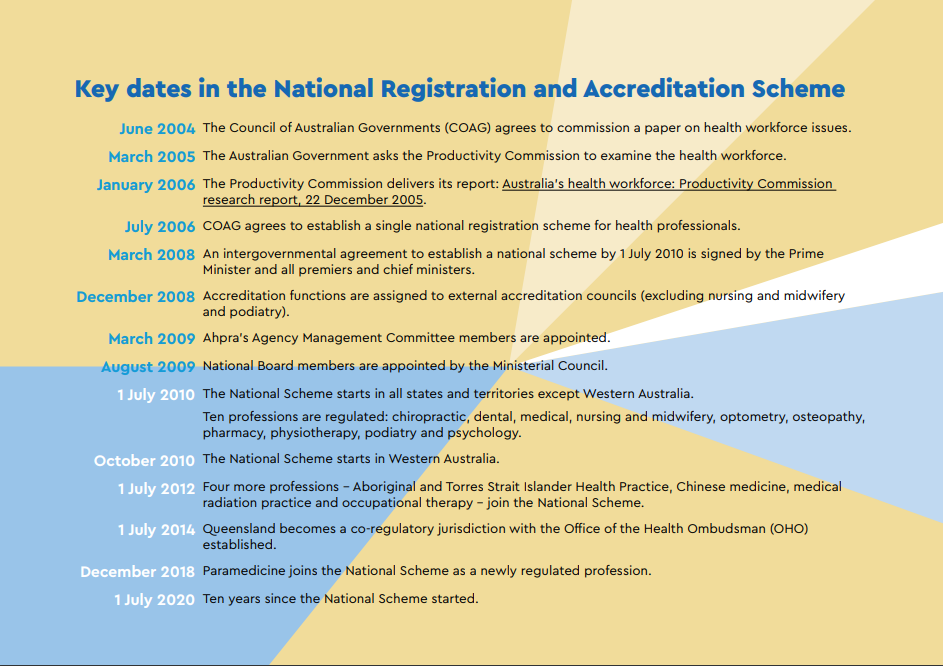
The National Registration and Accreditation Scheme (the Scheme), encompassing the Australian Health Practitioner Regulation Agency (Ahpra) and 15 National Boards, began in seven of Australia’s eight states and Territories in on 1 July 2010, with the eighth jurisdiction joining the scheme in October of that year. The Scheme came about after the Australian Government asked the Productivity Commission to examine health workforce pressures and propose solutions that would guarantee the continued delivery of quality healthcare over the next decade.
The report raised a number of issues with regulatory arrangements (duplicated registration and accreditation bodies in each jurisdiction, for each profession) including limited workforce mobility (eg a doctor in Victoria couldn’t assist in response to floods in Queensland without first becoming registered in Queensland) and a need to improve public safety by addressing identified failures in professional practice (eg instances of practitioner neglect, repeated misconduct or negligence and the subsequent media attention).
There are a number of features that make this single regulation system Scheme unique in an international context:
- The National Law focuses on public safety, health workforce and access to service objectives due to the Scheme’s inception as an examination into the health workforce and recognition that regulation occurs within the health workforce context.
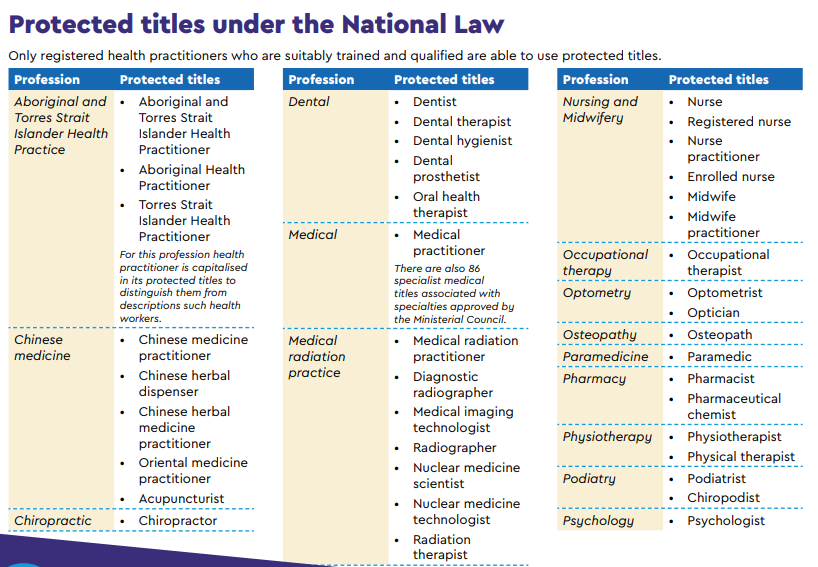
- The National Law regulates titles rather than scope of practice, with a very limited number of specifically restricted acts.
- The governance of the national scheme includes profession specific National Boards working in partnership with Ahpra, Accreditation Authorities and governments.
- We regulate the only profession I know of internationally that is defined by race in the registration of Aboriginal and Torres Strait Islander Health Practitioners.
Practitioner mobility
The Scheme allows Australian health practitioners to be registered once with Ahpra and be eligible to practice in any location in the country. We have over 800,000 registered practitioners across 16 professions. This approach allows the health workforce to be far more flexible and responsive to changing needs and reduces the cost and red tape burden for practitioners who would otherwise have to pay for and maintain registration in multiple jurisdictions if, for example, they wished to provide country-wide telehealth services or assist in another jurisdiction. While the pre-2010 arrangement included mutual recognition in many cases, the costs and professional standards required for registration varied and made mobility across jurisdictions difficult.
Scope of practice and title protections
The pre-2010 health practitioner registration and regulation approaches in Australia tended to rely on profession specific regulation by statute and restrictions on practices and titles. This approach did not lend itself to being responsive to the changing needs of the community or health practitioners.
Under the Scheme, National Boards focus on title protection rather than the scope of practice of registered health practitioners. There are broad guidelines about scope of practice provided by practice standards and codes of conduct, but the more flexible approach better allows health practitioners to respond to changing models of care.
Getting everyone involved
While the Scheme provides a single place for practitioner registration, it also involves 15 National Boards, one regulatory agency (Ahpra) and a suite of independently exercised accreditation functions.
This single regulation system allows for a much higher level of cross-professional collaboration than is often seen in other countries. The National Law requires National Boards to consult each other, but the Australian model also allows National Boards and Ahpra to work together across a range of topics, with a focus on consistent regulatory standards both geographically and from profession to profession.
It also means that means that community members and stakeholders have a single point of initial contact – Ahpra - when they need information or wish to provide feedback about the services being provided and ensures more efficient pathways for Ahpra to ensure that they are hearing from interested groups in the community.
There are several groups set up to formally provide feedback to the Scheme from stakeholders and community members including the Community Advisory Council, Professions Reference Group and Education Provider Reference Group.
How we were able to respond to the COVID-19 pandemic
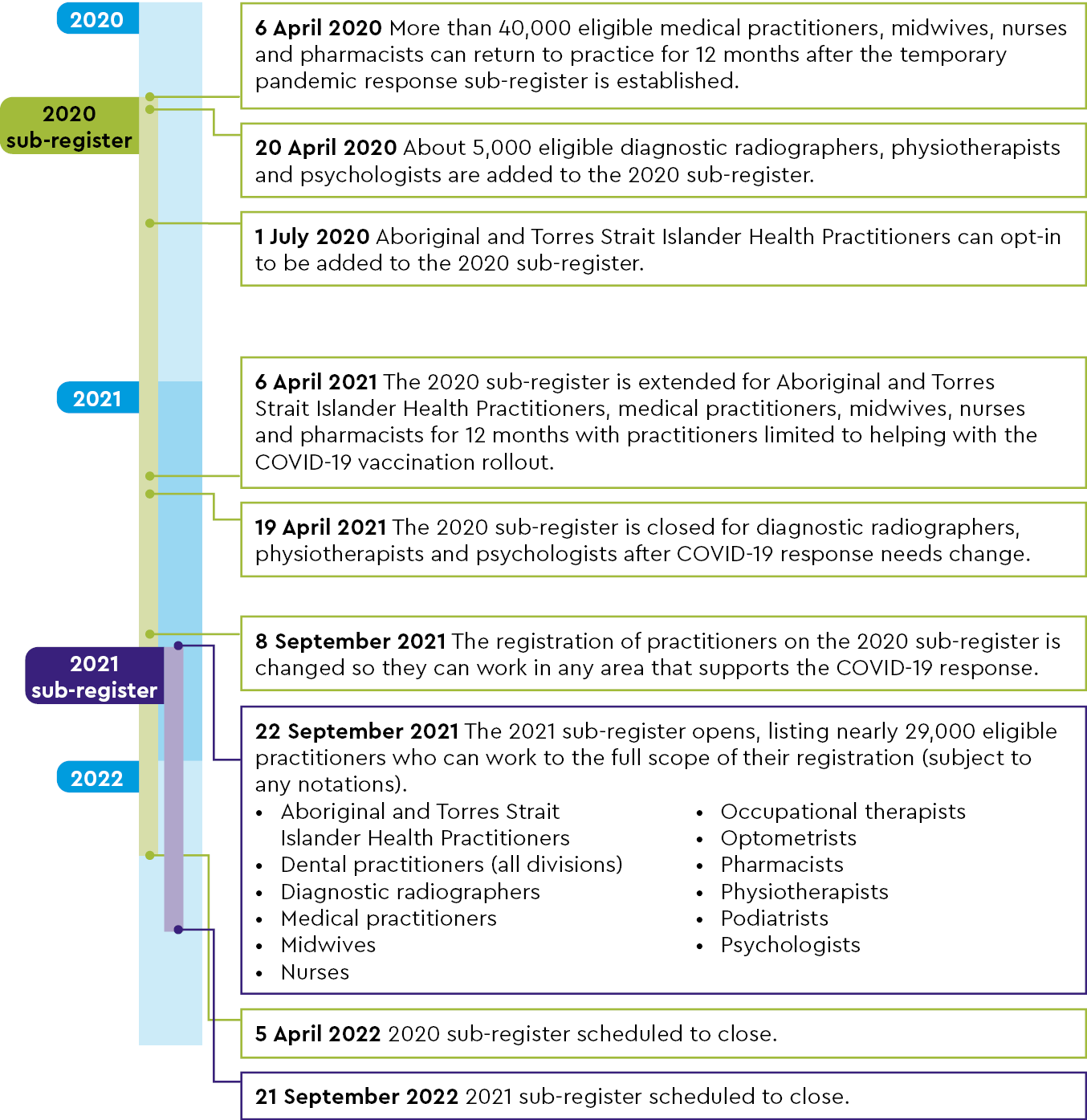
In addition to flexibility provided to registrants, students and accredited course providers we contributed directly to the surge workforce needs. During 2020 and 2021, Ahpra was able to rapidly stand up a pandemic response sub-register that had health practitioners who were in good standing and had stopped being registered in the last two years. This allowed jurisdictions to access staff with proven competency to provide health care more generally as existing systems were under strain, as well as COVID vaccinations and contact tracing.
Having a single register of 16 professions allowed this to be done in a careful, central way and reduced the risk of poor-quality information or lack of communication between regulators causing problems in an already stressed system.
While there are drawbacks to a single regulation scheme in Australia – the size and complexity can be unwieldly and make responding promptly to changing environments a challenge – after ten years of regulation in Australia, the public and the health workforce are clearly reaping the benefits that are unique to this model of regulation.